Browsing Insurance Coverage For Drug Rehabilitation: What You Need To Know
Browsing Insurance Coverage For Drug Rehabilitation: What You Need To Know
Blog Article
Web Content By-Woodward Knudsen
Picture browsing insurance policy coverage for Drug rehab as trying to assemble a complex challenge. Each item stands for a various facet of your policy, and the difficulty depends on aligning them perfectly to ensure comprehensive coverage.
Comprehending the complexities of insurance can be challenging, however fear not, as we break down the crucial parts that will certainly encourage you to make educated choices and safeguard the support you require.
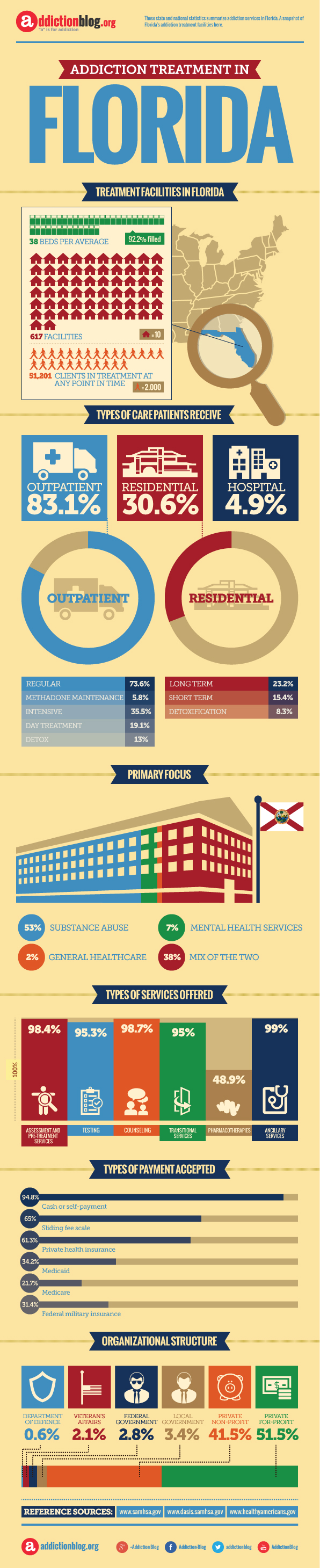
Comprehending What Is Drug Addiction Treatment in Florida is the first step in your journey to making the most of the advantages offered to you.
Comprehending Insurance Coverage Insurance Coverage Essential
To grasp the fundamentals of insurance policy protection for Drug rehabilitation, begin by recognizing exactly how your plan features. Check out whether your insurance policy strategy consists of psychological health and substance abuse advantages. Examine if there are any specific requirements for coverage, such as pre-authorization or recommendations.
Comprehending your insurance deductible and copayment duties is essential. Familiarize on your own with the regards to your policy, like in-network companies versus out-of-network companies. Recognizing the extent of protection your insurance uses for various types of therapy programs will certainly help you intend properly.
Track any kind of restrictions on the number of sessions or days covered to avoid unexpected costs. Being Read Alot more in understanding your insurance policy can make a considerable distinction in accessing the treatment you need.
Trick Elements for Coverage Resolution
Comprehending crucial factors that identify coverage for Drug rehabilitation under your insurance coverage is important for browsing the process properly.
The primary aspects that affect insurance coverage include the type of treatment center, the certain services given, the duration of treatment, and whether the center is in-network or out-of-network.
In-network facilities are typically much more budget-friendly due to the fact that they have actually worked out prices with your insurance company.
Additionally, your insurance plan might need pre-authorization for treatment or have details standards that must be met for coverage to be authorized.
It's important to assess your plan thoroughly, understand these vital aspects, and communicate effectively with your insurance policy service provider to guarantee you optimize your coverage for Drug rehab.
Tips for Maximizing Insurance Coverage Conveniences
To maximize your insurance benefits for Drug rehabilitation, it's important to be positive in checking out means to optimize coverage. Right here are some ideas to help you maximize your insurance coverage benefits:
- ** Review Your Policy **: Recognize what your insurance policy covers and any constraints that may use.
- ** In-Network Providers **: Choose rehabilitation facilities and healthcare experts that are in-network to minimize out-of-pocket costs.
- ** Utilize Preauthorization **: Acquire preauthorization for therapy to make certain coverage and avoid unforeseen expenses.
- ** Appeal Denials **: If an insurance claim is denied, do not wait to appeal the decision with extra information or assistance from your doctor.
Read Home as a compass overviews a ship via treacherous waters, comprehending insurance policy protection for Drug rehab can navigate you in the direction of the ideal therapy path.
By knowing the basics, crucial variables, and suggestions for taking full advantage of advantages, you can steer clear of challenges and get to the safety of recuperation with confidence.
Allow your insurance policy coverage be the directing light that leads you towards a brighter, healthier future.